We often speak admirably about the human spirit — resilience, passion, resolve — and shy away from our fragility and mortality, especially when it concerns viruses. After all, what could be more terrifying than the idea that our bodies are deteriorating because of something unseen? And what could be worse than knowing there was no way to get better?
Such was the reality for patients afflicted with human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), a chronic, life-threatening condition that previously was a death sentence. And while HIV/AIDS patients languished physically, they also suffered emotionally, facing social isolation and scrutiny. Indeed, few other diseases carry as much cultural significance as HIV; homosexual, African-American and immigrant patients faced unprecedented levels of discrimination during the 1970s and 80s. Today, patients continue to face the stigma associated with HIV despite effective noncurative treatments and prophylactic agents.
Biologically, HIV is a single-stranded, positive-sense ribonucleic acid retrovirus that causes AIDS. HIV preferentially infects and kills the body’s immune cells, including helper T cells, which help to mediate the body’s ability to respond to infections. When the body loses these critical cells, patients become more susceptible to the types of viral, bacterial, and fungal infections that healthy people do not normally get sick from. This pathobiology raises two questions: how does HIV infect these cells? And why are only immune cells affected?
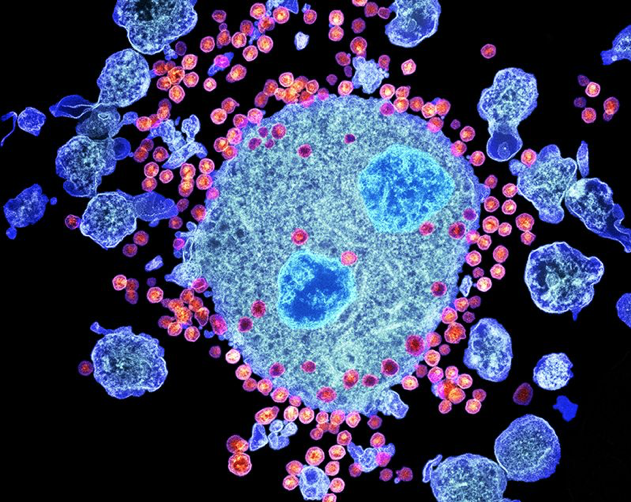
HIV exhibits a unique tropism, a preference for infecting certain cells in the body. This tendency is caused by special proteins on the surface of HIV particle, called envelope glycoprotein 120 (gp120), which interacts with proteins on the surface of helper T cells, including CD4. You can think of gp120 as a key that is able to fit into the lock, CD4, which allows HIV to infect helper T cells. Other proteins on the surface of helper T cells, such as CCR5 and CXCR4, are also important for HIV infection and permit the virus to enter the cells, like a molecular doorknob.
Once in the cell, the HIV particles break down, releasing its viral genome and proteins. It then copies and pastes its genome into the cell’s genome and co-opts the cell’s own proteins to make more HIV particles. These particles are released into the bloodstream to infect more cells. These steps are discrete and involve the participation of both HIV and human proteins; one can imagine how interrupting anyone step can prevent the production of HIV particles.
In fact, this idea of blocking intermediate steps is how the first HIV antiretroviral therapies (ARTs) were initially conceived during the 1980s and 90s. Now, these drug therapies are often used in combination to control HIV viral levels in patients and prevent the transmission of HIV to romantic partners and healthcare workers. Despite incredible improvements in patient survival and quality of life, patients experience a lifetime of drug side effects, including liver toxicity and neuropathy, and these multi-drug regimens are by no means a cure — until now.
Last week, physicians and researchers in the United Kingdom reported that a patient had been “cured” of HIV, the second such report in the history of HIV. The patient, who is only identified as the “London” patient, was diagnosed with HIV in 2003, which was managed well with ART. In 2012, the patient was sadly diagnosed with advanced Hodgkin’s lymphoma, a rare blood cancer that affects white blood cells called lymphocytes, and received a special bone marrow transplant (BMT) as part of his treatment.
So what is BMT? All blood cells in the body—erythrocytes (red blood cells), macrophages, B lymphocytes, and T lymphocytes, including T helper cells—are made in the bone marrow. In lymphoma, the bone marrow produces too many abnormal lymphocytes, so treating lymphoma involves eradicating these abnormal cells and their precursors. Unfortunately, our best treatments, chemotherapy and radiation therapy, are unable to distinguish between healthy cells and diseased cells, and healthy bone marrow cells are destroyed in the process. This would be analogous to trying to use a flamethrower to weed a garden. After clearing the bone marrow, BMT is often needed to help the body regenerate blood cells.
In this case, the London patient received a BMT from a donor who had a rare mutation in CCR5 (dubbed CCR5∆32) that prevents CCR5 from being produced. CCR5 is one of the helper T cell proteins that permits HIV infection, and individuals with this mutation have been found to be more resistant to HIV infection. 18 months after receiving this special BMT, the London patient was found to have undetectable HIV levels. Could BMT cure HIV?
These are incredible and promising findings, but BMT is not without its risks and complications. In addition to requiring daily immunosuppressants, which disrupts the immune system in a way similar to HIV/AIDS, the London patient experienced dangerous side effects, including grant-versus-host-disease, where cells produced by the donor’s bone marrow attack the body’s tissues. There is also insufficient evidence to suggest that such approaches are better than ART, which are the current standard of care.
In spite of these limitations, scientists, physicians and HIV patients alike are excited about the prospect of using BMT to “cure” HIV. Perhaps in the coming decade, society as a whole will recognize the human experience of HIV patients and celebrate the spirit of its survivors.