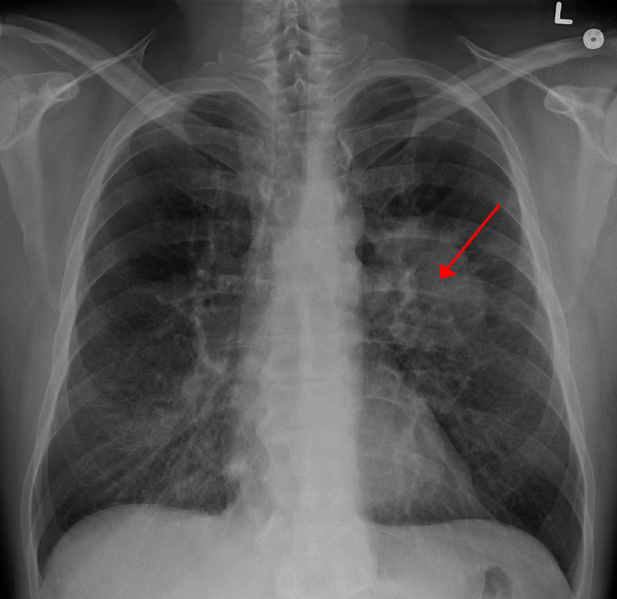
Most of us know from our high school health classes that we should avoid smoking because it can cause lung cancer. Many students were presented with disturbing visuals that compare healthy lungs with a smoker’s lungs or were shown other such scare tactics, but the message is always the same: lung cancer, which can be caused by smoking, is often fatal. Now, although smoking still has the same negative effects on your health, a new treatment for lung cancer involving the immune system might be the key to decreasing the mortality rate of lung cancer.
This new treatment combines more traditional chemotherapy with a form of immunotherapy, a way of boosting your immune system to fight back against disease. Immunotherapy is not a novel idea, but its use in treating lung cancer was examined in a study was done by oncologist Dr. Leena Gandhi and her team at the Perlmutter Cancer Center at New York University Langone Health. Their goal was to assess the effectiveness of this promising update in cancer-treatment protocol. The study focused on people with an advanced form of non-squamous non-small-cell lung cancer, the most common type of lung cancer. The study was diverse, with over 600 participants from 16 different countries ranging from their 30s to their 80s. The diversity in subjects helped control for variation in lifestyle or age, which could impact death rates.
The immunotherapy treatment is called pembrolizumab. This drug is a checkpoint inhibitor, which means that it stops the body from controlling certain immune system response cells. Essentially, the drug causes a boosted immune response in the body and kills off unwanted cells. Unwanted cells would, of course, include cancerous cells, which is what makes this form of treatment so effective.
There is a great need for new lung cancer treatment options, especially for late stage cases. Chemotherapy alone is only moderately beneficial, according to Dr. Gandhi. However, when chemotherapy is combined with immunotherapy, there is a significant increase in survival rates: the study found a 69.2 percent survival rate after twelve months in the group that received both immunotherapy and chemotherapy and a 49.4 percent survival rate among those who received chemotherapy alone.
Dr. Roy Herbst, who is the Chief of Medical Oncology at the Yale Cancer Center, has hypothesized that the combination is so effective because the chemotherapy exposes some of the cancerous cells so the body can respond and fight back; when this process is combined with an increase in that fight response, it effectively decreases the number of cancerous cells in the body.
Whether or not Dr. Herbst’s hypothesis is correct, the ongoing study has shown promising results so far. Results will continue to be generated as the two groups proceed in their courses of treatment.
Studies like Dr. Gandhi’s also raise ethical concerns about what researchers should do if there seems to be a clear difference in survival rates between two different groups in a study. Is it ethical to keep people with advanced lung cancer on chemotherapy alone if it is strongly suspected that their chances of survival are better if they were receiving both chemotherapy and immunotherapy? Questions like these will remain crucial as the study progresses.
For now, remember your high school health classes and try to keep your lungs smoke free!